
A right lower limb motor deficit was observed at 11:50 a.m. After an abdominal ultrasound, urinary retention was observed and a bladder catheter was inserted (residual volume: 1100 ml). of the 6th post-operative day, more than 70 h after the removal of the epidural catheter, the patient complained of acute and severe low-back pain, radiating to the right inferior limb, and paresthesia there was no motor impairment and she was treated with analgesic drugs without any improvement.
The following day, the patient remained hospitalized without any complications and the two babies were admitted in neonatology.Īt 06.00 a.m. PCEA was discontinued 2 days after the operation and the epidural catheter was removed on the 3rd day, 12 h after the last Dalteparin administration. Four hours after the operation, the urinary catheter was removed, the patient began to stand up and to take care of the newborns.
EPIDURAL SITE PAIN YEARS LATER PLUS
ketorolac 30 mg/day and oral tramadol 30 mg plus acetaminophen 1000 mg/3 times/day).

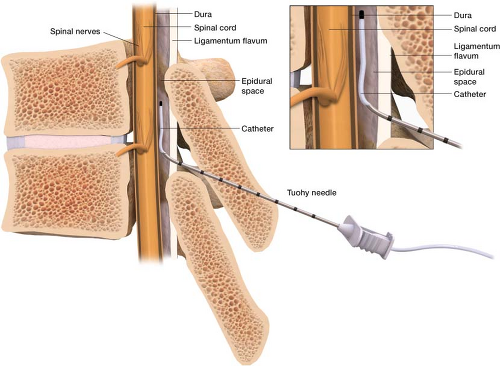
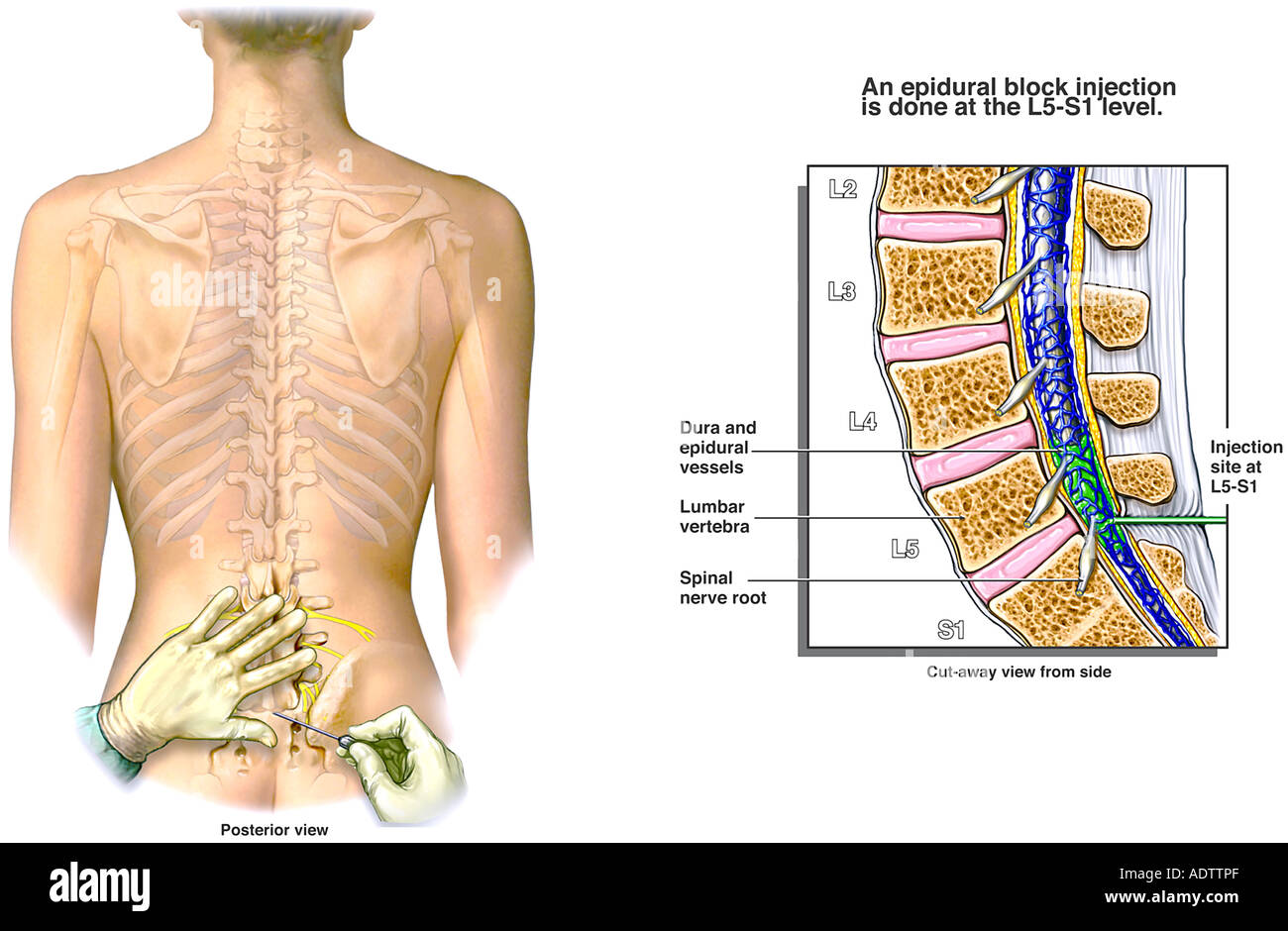
The operation was carried out routinely and multimodal pain therapy was started (Patient Controlled Epidural Anaesthesia - PCEA - with chirocaine 0,15% plus sufentanil 0,5 mcg/ml, 4 ml/h i.v. Preoperative coagulation parameters were within normal range (Platelet count 120.000 per microliter of blood Prothrombin time 12 s, Partial thromboplastin time 30 s, fibrinogen 540 mg/dL, INR 0.90). Braun Perifix® epidural set), placed during a single attempt. The patient underwent a planned caesarean section under double-space CSE anaesthesia, using a 25-gauge atraumatic spinal needle at level 元-L4 and an 18-gauge Thuoy needle at T12-L1 (B. Considering 4 days of immobilization in bed, low molecular weight heparin (Dalteparin© 2500 UI one per day) was administered. The patient suffered from unstable insulin-dependent type I diabetes and sciatica. In order to achieve the best clinical result, we stress the importance of a timely diagnosis and prompt surgical treatment.Ī 44 year-old pregnant nulliparous, weight 70 Kg, height 172 cm, BMI 23.7, at 34 weeks of a twin gestation, obtained by “in vitro” fertilization, was admitted to the General Hospital of Massa, complaining spreading pricking and lower limb edema. The possibility of the delayed onset of a spinal epidural hematoma in a pregnant woman who undergoes epidural anaesthesia in labour must always be taken into consideration. The patient was moved to the Neurosurgical Department and underwent decompression surgery. An MRI scan showed a dorsal epidural hematoma. Symptoms were reported 5 days after surgery and 72 h after removal of the epidural catheter. We reported a case of a 44-year-old woman who underwent a caesarean section for a twin pregnancy during which a delayed dorsal spinal epidural hematoma occurred. Delayed clinical presentation of spinal epidural hematoma is even rarer and insidious. Epidural hematoma usually becomes evident within a few hours of the procedure. Spinal epidural hematoma is a rare but serious complication of epidural anaesthesia and neurological impairment.


 0 kommentar(er)
0 kommentar(er)
